Welcome to this bumper edition of the CFSG newsletter. It is ‘bumper’ because it is rather overdue. But, like the best things in life, hopefully worth waiting for! In this edition we are reflecting on the family weekend and conference that was organised in Septembers last year. The CSFG committee have also taken time to write a short introduction each so you know a little more about who is who. Don't miss the rare opportunity to hear Dr Gail Deuce, one of our committee. She is leading seminars in Derby on educating children with Charge Syndrome on July 29th – details on page 8.
In addition, we focus on two remarkable people in the Charge syndrome Community – Lesley Rogers who last year won the Sense award ‘Volunteer for the Year’ and Carl Bradley, a young man with Charge syndrome who has graduated from the London Academy of Music and Dramatic Art and is setting up his own business.
In the final three articles, Dr Kirk explains more about the Birmingham Charge clinics, Lyn Ayer, from the Oregon Deafblind project outlines her guide to overcoming feeding difficulties and Claire Vincent shares her guide to writing an EHCP.
Lastly, it leaves me to say, with very mixed feelings,that I have decided to take a step back from being editor of this newsletter. I have thoroughly enjoyed expanding my knowledge of the CHARGE syndrome community through this role, however there are some personal issues that need to take precedence over the coming months. Thank you so much to everyone who has submitted articles and given encouragement over the last 2 ½ years. If you enjoy the newsletter please consider volunteering for the role of editor. You can email me (estbu@hotmail.com) or Simon (si_howard@hotmail.com). There is lots of support available.
Editor: Esther Freeman (estbu@hotmail.com)
Page 3: New logo – Creating the Concept by Claire Vincent. Page 3-8: Committee changes and Introductions.
Page 8: Educating children with Charge Syndrome. Page 8-9: ‘We are Family’ by Esther Freeman.
Page 9-10: ‘Sent to Coventry on an Amazing Road’ by Frances Concanon. Page 10-11: Lesley Rogers – Volunteer of the Year.
Page 11-12: Carl Bradley – This is your Life!
Page 12: Charge Clinics in Birmingham by Dr Jeremy Kirk. Page 12-17: A Guide to Feeding by Dr Lyn Ayer.
Page 17-20: Claire Vincent's guide to EHCP.
2

Claire designed the new CFSG logo. The concept behind the design was to use a colour spectrum that reflected the diversity of CHARGE syndrome. The logo uses bright colours and a simple clean font that are easy for people with visual impairment to see. The logo is modern and fresh giving CFSG a great new brand identity.
At the Family Weekend and conference in September 2016 we sadly said goodbye to Lydia Howarth who had been Chair of the CFSG for many, many years. We are very grateful for her role in organising us all and being so proactive in making things like the family weekends happen. She gave up so much of her time for the benefit of us all and we want to say a huge thank you…
Frances Concannon also stepped down as Secretary although she is staying on the committee for 12 months to give support to all the new members. Again we would like express deep gratitude to Frances for all her careful minuting of meetings, work behind the scenes, organising of family days and, not least, securing the Jeans for Genes grant which enabled our conference to go ahead last year.
Steven Ho kindly stepped up to be the new Chair and Leanne Howie as the new Secretary. Also new to the committee is Myriam Lantrade. You can read more about us all in the ‘mini bio’ sections below.
Steven Ho – Chair.

regular on the group!
My name is Steven Ho and I am, like most of the Charge Family Support Group committee, a parent to a child with CHARGE. My daughter Eva will be 3 in April and I’m pleased to say she is confounding the limited expectations she was set during her early life. My professional background is in computing but I currently work at a small cancer charity as a General Manager looking after volunteers, supporting patients, doing fundraising, whatever needs to be done! For those of you on the CHARGE Facebook group you may have seen me post from time to time but you are more likely to see posts from my wife Jemma, who is a
My sincerest thanks must go to my predecessor, Lydia Howarth, who did a fantastic job as Chair. I look forward to continuing her great work and hopefully utilising my
3
professional experience to benefit the charity. If you ever see me at a CHARGE family day please do come up and say hello - my wife says I am always frowning but I’m not as grumpy as I may look, promise!

Me (left) with Rob from Oz and Tim from USA
My daughter Jess was born nearly 17 years ago. Access to information was nothing like today but she was diagnosed with CHARGE at 6 weeks. Having contacted Sense we discovered there was a family day so the first trip out of hospital at 12 weeks was to this. We met 6 other families who made us very welcome. A few years later with Carol Thomas becoming Chair I started writing the newsletter. Between us the group developed with Carol running a northern family day and me a London one. It was at one of these I convinced Lydia and
Frances to join us and form a committee. Jeremy Kirk and Gail Deuce came on board as well at the same time.
Over the years the committee has developed and grown. I have represented the group at a number US conferences with poster presentations, done joint research with Sense and been involved with the organisation of Sense's CHARGE conference in 2011.

Leanne is mum to two children, Tyler (5) and Robyn (4) who has CHARGE. She is one of our Scottish Committee members and is based in Dundee. Leanne is currently training to become a Regional Makaton Tutor as she uses Makaton at home to communicate with Robyn who is non verbal. She organised and ran a Signing Santa Grotto in Dundee last Christmas that was very well received by local children with many varied conditions. She hopes to continue to bring signing into much wider use in her local community over the next year. Leanne is the Secretary for the CFSG committee.
4

I am the fundraising officer for CHARGE FAMILY SUPPORT GROUP and have been on the committee since 2011 after I was diagnosed in 2010 at the age of
40. This group has become part of my life now and I will continue to be a part of it for the foreseeable future.
When not doing charge related stuff I am a Facilities manager for the NHS and a full time foster carer for my local authority with my wife Karen.

Hello, I am Peter Hughes, Honorary Treasurer of the charity. I live in Sale Cheshire, part of Greater Manchester. I became involved with Charge when my granddaughter was diagnosed with the syndrome in 2010.
My role as treasurer started at the National Family day in Coventry, 2014. The charity needed a treasurer, I volunteered for the role, and was happy to help. What I do is I manage the finances for the charity:
issue
each month bank any cash donations,
arrange raising a cheque for any expenditure. Another committee member then has to countersign cheques which I
check all expenditure and income against the bank statements
each month prepare an expenditure and income return for the committee. That includes the amount in our current and deposit accounts. This is so that the
committee knows what is available for authorising activities.
annual preparation of the balance sheet for the financial year ( April to March)
prepare and submit our returns to the Charity Commission on behalf of the charity
Jeremy has been Medical Advisor to the UK CHARGE Syndrome Family Support Group (CSFG) for the last 25 years. He has lectured extensively on CHARGE syndrome including in Germany, Denmark, Australia, Romania and also at 9 of the 12
USA meetings. Jeremy is a paediatric endocrinologist at Birmingham Children’s
5

Hospital and honorary Professor at the Universities of Birmingham and Wolverhampton. He is also Clinical Director of the NIHR Clinical Research Network for the West Midlands.
There are now multidisciplinary CHARGE clinics established at Birmingham Children’s Hospital and also University Hospital Birmingham.
Claire is mum to 5-year-old Mia who was diagnosed with CHARGE at birth. Mia has two brothers Oscar, age11 and Oliver, age 8. They live in north London with dad Rob. Claire became a CFSG committee member in September 2016 and has been

helping with developing the charities branding. Over the past year Claire has been given talks to parents and health professionals about deaf and MSI children in mainstream school at the Charge Family weekend in Coventry and for Auditory Verbal UK.
In 2013 Claire and her husband Rob set up a media production company called Popla Media, where they make films, take photographs and tell stories for creative companies and charities. They are particularly interested in working with companies who want to make a difference to people’s lives. Claire is
about to start a film project called ‘Stories like me’ which will explore how deaf children and young people find their identity in a world where they are barely visible?
I am a teacher for children with multi-sensory impairment. I work three days a week for a London borough. This allows enough time for me to do independent work, focusing on what I love best- working with children and young people with CHARGE.

I met my first child with CHARGE over 20 years ago and became hooked! Over the years I have been very fortunate to work with lots of children with CHARGE. More recently I have undertaken
a PhD, researching the education of learners with CHARGE. I joined the CHARGE
Family Support Group some time ago (I can’t remember how long but Simon will
6
probably know), and am on the committee to give professional advice and support where I can.

My name is Lianne and I'm from Edinburgh. I have two lovely children, Bailey age 5 and Kerr age 3. My life changed significantly when Bailey was born (as it does with a CHARGER)! I joined the family support group to find out more about CHARGE and to meet others in the same situation. At our first family weekend I volunteered my services to be on the committee as we didn’t have a Scottish representative. Leanne and I organised the first ever Scottish family day in 2015 and are hoping to have another one soon.
Formerly Secretary of the Group, I am mother of William, who will be 18 in March

(2017) and Tom (now 14). Best thing about my family
– I am the only girl so get to be ‘Queen Bee’ all the time. Worst thing about my family – I am now the shortest person in it! I work at a boys’ secondary school in Kent as a pastoral manager, but also have experience in marketing, PR and event management. I also make and sell my own range of jewellery. I am passionate about supporting others and am a real “people person”.

I am the mother of Theo who has CHARGE Syndrome. Theo is the oldest of 3 and is 9 years old. He has 2 little sisters Margot (7) and Noemie (2). We have been living in South West London for 5 years now. I am working as a Product Director in an international financial technology company in London.
Me and my husband are originally French and moved to the UK 13 years ago. I am sure
7
you can guess which London team we are supporting…..We are Gunners through and
through. Theo loves going to Emirates with his dad.

I have two children – Jasmine is 7 and has Charge Syndrome. Her brother, Ben, is 5. When I am not busy with them, I work as a nurse in the local hospital and I’m also Chair of the PTA at my daughter’s Deaf school. We live near Derby and love heading out to the Peak District when we have a free weekend. I have just stepped back from editing the CSFG newsletter as I need to focus on improving my BSL to keep up with Jasmine!
There is a rare opportunity to attend an afternoon of seminars with Dr Gail Deuce, MSI consultant and leading educationalist in Charge Syndrome; 29th June 12.30-15.30 followed by questions. The sessions will cover:
• Introduction to Charge Syndrome
• Learning characteristics of children with Charge.
• Teaching strategies for children with Charge.
• Responding to the Charge behavioural phenotype.
It will be relevant to teachers, TA's, intervenors, parents, carers involved with a child with Charge Syndrome at any stage in their education. Certificates of attendance can be given.
It will be held at the: Karten Centre, Royal School for the Deaf, Ashbourne Road, Derby, DE22 3BH. £25 but discounts available for families / group bookings. Email estbu@hotmail.com if you'd like more information or to attend.
Did the composers of the Sister Sledge hit “We Are Family” realise in 1979 what a hit it would become and its continuing impact as a song celebrating solidarity right up to the current day? It was also 1979 when the term CHARGE Association was first used but it took 25 years before Dr Conny van Ravenswaaij identified the gene CDH7, and formally defined CHARGE Syndrome. CHARGE is a rare syndrome that affects all the body’s senses, and being able to connect with our wider CHARGE family to gain support and knowledge is incredibly powerful.
8
On 16 September, over 40 people including scientists, clinicians and MSI teachers attended the first UK CHARGE Professionals’ Day in Coventry. They listened to eight different presentations from national and international speakers spanning: basic science, clinical and MSI management issues. According to organiser Prof Jeremy Kirk, feedback was universally positive, and as one delegate stated: ‘I acquired such detailed medical knowledge which I can now utilise to improve my practice.’ It is hoped to hold these meetings regularly in the future.
The following day families from the CHARGE Family Support Group arrived. We came as families from all over Britain, and left with a fresh sense that we also belonged to a wider community of people who understood our struggles and achievements.
First thing in the morning the fantastic Leisure Club, run by Sense, went into full swing. The children and young people had an amazing time – as evidenced by the photos! Our children are complex and it can be difficult to leave them in new situations. However, Lisa sums up the experience beautifully: ‘Leaving Violet with the Sense team was a big thing for me and her, as she doesn't do well with strangers. Well she proved me wrong and had lots of fun without me! Thanks so much to the wonderful Sense team, especially to Becki the midwife!’ An enormous thank you to Sense for their expert care, and also to Jeans for Genes for their generous grant which made the Leisure Club possible.
Whilst the young people played, the adults learnt from the incredible expertise of professionals who offered their insights during four different seminars. There was also plenty of opportunity over coffees, lunch and the evening meal, to meet, network, share stories and gain insights and encouragement. As Violet’s Dad, Shaun, comments: ‘What a great community all the CHARGE families make. A fantastic day of fun, learning and meeting.’ I am sure many also echo Faye, Luca’s Mum who reflected: ‘Absolutely amazing. It was my first ever family conference day, and as soon as I walked in I found it very emotional. Made me feel like I'm not on my own’.
The CHARGE Syndrome community in the UK is so grateful that we can come together at events like this and connect with our ‘wider family’. Thank you Sense for all your support!
(This article was first published for Sense Magazine, Autumn 2016.)
I took Esther up on her offer of a copy of Marina Sanchez’s book of poetry, in return
for the following. A small price to pay for a wonderful collection of poems.
I have to be honest, sitting in my office on Friday 16th September watching the roads on the AA traffic map turn red in front of me, my heart sank. Two weeks before I had started a job that was proving as mentally and emotionally exhausting as it was stimulating. I was tired! A weekend at home with the family felt much more appealing.
9
The drive to Coventry from Kent could have been worse. I got there in the end! Food, beer and a reunion with a few good friends and I started to feel better. From that point on the weekend – as I knew it would – started to work its magic….
New friendships made and old ones renewed, serious and frivolous issues discussed and debated with equal rigour and good humour, many questions answered and a few still needing answers; and children, children everywhere, running, laughing, signing, sleeping, exploring, playing – tough, indomitable and inspiring.
I have been privileged for the last few years to have been close to the beating heart of The CFSG, as Secretary of the Group. The Committee is a wonderful collection of generous, supportive, hardworking people with experience and talents that have allowed the Group’s activities and ambitions to grow. Several people asked if I was relieved to stand down. Not relieved – proud of what I have helped to achieve and happy to hand the baton on to someone new (Leanne, you will be great, but I’m only an email away if you need me!). I know the Committee will go from strength to strength.
With informed and informative presentations from World-leaders in their respective fields, amazing volunteers and professionals who flocked to support and learn more about our children, good food and plenty of time to chat and reflect with all our wonderful families, the Coventry weekend ensured I went home re-energised, refreshed, reinvigorated – you could say re-CHARGEd.
We are very proud to give a ‘shout out’ to Lesley Rogers who is a member of the CFSG. Lesley won a prestigious award from Sense last year. This is what their magazine Talking Sense had to say:
‘Lesley is mum to Ruby who is deafblind, and this year volunteered to co-chair Sense's Public Enquiry into play opportunities for young children with multiple needs – working alongside Lord David Blunkett and colleagues from the Public Policy Team. She also appeared on the Today programme on BBC Radio 4 and contributed an enormous amount of the project.’
10
Well done Lesley. As a group we are incredibly grateful for the work you have done in highlighting the issues around equal play opportunities and advocating for our children.
Carl is 30 yrs old and wanted to share his story with the Charge community in the UK in the hope that we would be encouraged about what can be achieved and to give hope for the future.
Carl Bradley was born with CHARGE syndrome. His symptoms included hypotonia, feeding difficulties and hearing loss which resulted in a number of major operations and years of intense speech therapy. As an infant, he struggled to feed from a bottle and received special support to teach him to walk and talk. He was not able to walk unaided until the age of three and had to wear a cycle helmet at playtime and PE as he would easily fall and injure himself.
Despite these obstacles, Carl was determined to achieve and strived to continue in mainstream education with 1:1 support. At 11 years old Carl won the Child of Achievement Award alongside his sister. They were the first siblings to achieve the award which is presented to children who have battled to succeed against the odds.
It was at the age of 12 that Carl found his love of drama as a student of Jane Ashdown, winning awards and passing LAMDA (London Academy of Music and Dramatic Art) exams for his acting. In
2003 he decided that he wanted to turn his passion into a career and became a student teacher. In
2004 Carl joined Jane’s DramActive classes at Norwich High school. He continued to climb the LAMDA grades and graduated as a speech and drama teacher, all whilst working part time at Tesco in order to save money to travel the world.

Carl said: “I did this with my determination to succeed but I could not have done it with the support of my family and friends, Jane Ashdown, the teachers and parents at DramActive and Norwich High School for Girls. It is to these people that I am eternally thankful to.”
“I wanted to tell my story so that
hopefully I can inspire the
children I teach and anyone else that has any difficulties. I wanted to let them know
that it is ok to be unique and to never give up on your dreams. It doesn’t matter what
11
difficulties you have or where you come from if you want something go get it and never
give up. “
Birmingham now offers 2 dedicated CHARGE clinics; one for children and adolescents based at the Children’s Hospital, and also an adult service based at University Hospital Birmingham. Both of these clinics contain a number of different specialists in CHARGE syndrome, enabling us not only to provide better, holistic care, but also hopefully limiting the number of clinic attendances.
The paediatric CHARGE clinic at Birmingham Children’s Hospital (BCH) has now been running for several years; it is currently run every 2 months and sees patients from across the UK and beyond. At present the clinic consists of 2 paediatric endocrinologists, a general paediatrician, a speech and language therapist (SALT) and a representative from SENSE. With the opening of the Rare Diseases Centre at BCH in autumn 2017, being built through our Star Appeal (https://www.bch.org.uk/?q=newcentre) and the only centre of its type in the world to provide holistic care for children, the CHARGE clinic will be moving and also expanding, to include other specialties and also hopefully including representatives from the CSFG. Apart from providing high quality care for our patients, the Rare Diseases Centre will also offer improved facilities such as 12 clinic rooms, kitchens and suitable toilet and changing areas, sensory and “chill-out” rooms, and areas for the families to mix. We also will have the facility to perform high quality research to help improve the diagnosis, treatment and care of our patients and families
We have also been holding an Adult CHARGE clinic (the only one of its kind in the world) at University Hospital Birmingham (UHB) since early 2016. These clinics are currently held 3 monthly, and currently include an adult physician (endocrinologist), a paediatrician (paediatric endocrinologist (me)), a geneticist, and a representative from SENSE. It is hoped that we will ultimately move into the Adult Rare Diseases Centre which is also based on the UHB site, enabling us to expand the clinic to include other specialties. As with the paediatric centre this will not only provide better, holistic care for our patients and families but also reduce the amount of travelling and hospital appointments.
This article contains notes I took while at a feeding seminar, as well as my own experiences and reflections. There was a great deal of information shared at the
12
seminar — and so I had to pick and choose what I wanted to share. I wish I could share more!!
Feeding has always been of interest to me since it affects so many of our children. In November 2016 I was fortunate to attend a seminar with Dr. Suzanne Evans Morris as the presenter: “Moving from gastrointestinal discomfort to Inner-Directed Eating”. It was the word “Inner-Directed” that caught and held my attention. Any action that is “inner directed” needs no external motivation, and leads to the most satisfying outcomes. To me this indicated that feeding was — or should be — a very child- centered activity — and Suzanne’s focus was definitely on the child and family.
Suzanne Evans Morris, Ph.D., is a speech-language pathologist with New Visions near Charlottesville, VA ( http://www.new-vis.com/ ) She is known both nationally and internationally for working to identify and intervene with children who have feeding and pre-speech disorders. Her work is strongly family-focused. You can learn more — including looking at resources such as blogs, and videos from the Feeding Matters site: https://www.feedingmatters.org/video-library
Some “quick facts” relating to the gastrointestinal system:
Positioning while feeding matters a great deal. The gastrointestinal tract depends on the influence of gravity – and downward movement. What if a child is lying down and being fed? Does this make a difference? Yes. Can this be helped? If a child must lie down, a solution to this depends on what you are trying to do.
If you are trying to prevent reflux, then lying on the left side keeps more of the food in the stomach and prevents it from going back into the oesophagus.
If you are trying to make sure the food passes into the intestines – lying on the right will help get the food flowing from stomach to intestine.
Talking about reflux – what does this actually feel like? Many of us think occasional mild burning is all it is. For many of our children it is much more. Imagine having a really bad sore throat and how annoying and painful that can be. That is what happens when gastric juices from the stomach constantly come up and burn the throat. Think of how painful it is to eat when we have a really bad sore throat. Even liquids affect us.
The intestinal system is also known as the “enteric nervous system”. Consider it the “other brain” of the body. It has a large network of nerves, including the
large vagus nerve. It is also responsible for the release of several hormones such as adrenaline, noradrenaline, dopamine; and 90% of the chemical/hormone serotonin is found here. http://medical- dictionary.thefreedictionary.com/serotonin. Some of these hormones are related to stress – and it is why we really FEEL the stress — or the relief from stress — in our “guts”. Serotonin may control the intensity of pain, affect how a child sleeps or feels, and how efficiently the guts function. Once on a CHARGE syndrome foundation webinar on pain I heard that many children have what has come to be known as an “abdominal migraine”. I don’t know enough about this
– but it is worth asking questions of the medical community to see if these migraines connect to the facts in this segment. Link to CHARGE webinar: https://hknc.adobeconnect.com/_a772371855/p6p2t2fxsiq/?launcher=false&fc
sContent=true&pbMode=normal
There is a key role played by “good” bacteria in our GI system. Our cells and genes are actually outnumbered by bacteria 100:1. Microbes we acquire at birth
13
assist our bodies to resemble our parents, affect our immune systems, and have their own antibiotics. We even acquire these at birth. Babies born by C- section, or who do not breast feed miss out on essential microorganisms from the birth canal and their mother’s milk. Inevitably — although we don’t know details — medications and vaccinations will compromise some of these good bacteria. This is important to realize because many of our children who are deafblind may need the medicines for survival. We should always consider what we do – relating to this information. We may not have the answers, but sometimes our bodies “tell” us:
For example – Can we find out what side-effects there may be of medications
– on our hormones and good bacteria in the gut?
Another example – Is there any correlation of poorer immune systems and various immunisation shots given to children (and adults)?
Is there a way that we can counteract some of the less desirable results/side effects — e.g., by using probiotics?
New research on Melatonin suggests that not only does it help with sleep, but with reducing acid reflux, migraines, SAD (Seasonal Affective Disorder) https://www.youtube.com/watch?v=XNqKvwqDs60. We all know that sleep affects how we eat, how we feel — and how we behave. Think about children who are deafblind and have complex health issues who have no real way to tell us that their eating is being affected by lack of sleep. Also think about mothers who are afraid their child is going to choke in their sleep — and suffer from insomnia themselves!
As research is carried out, it is worth learning more about CRF (corticotrophin- releasing hormone) that is secreted by the hypothalamus, and controls the
secretion of the stress hormone (cortisol). In turn, this will suppress appetite and increase anxiety. Smaller quantities of CRF are made by certain white blood cells — which stimulates swelling or tenderness/inflammation, especially in the gut. CRF follows a 24 hour “rhythm” in non-stressful circumstances — highest in the morning around 8:00 a.m. and lowest overnight. A stressful experience, an infection, even exercise can trigger an increase in the hormone, to counteract the situation. If there is too much CRF in the system, appetite is suppressed. If this high level continues, it can lead to disorders such as anorexia, severe sleep disturbances, and clinical depression; and making certain inflammatory conditions worse — eg rheumatoid arthritis. In fact, it may
actually cause inflammation. Too little CRF may affect sleep, memory and concentration.
(1) http://www.yourhormones.info/hormones/corticotrophinreleasing_horm one.aspx; (2) https://www.ncbi.nlm.nih.gov/pubmed/2234606
Research still continues on how to control the levels of CRF. Medications may be life- saving (such as if too much acid is going into the lungs). But be aware that most medical procedures tackle the symptoms and may sometimes disguise them, but may not get to the underlying problem. The symptoms will usually come back when the medication is stopped. One must also consider the side-effects of medical interventions, including surgery. For example, after a surgery called fundoplication, a child is unable to vomit so will retch and gag instead.
Medication (eg Prilosec) usually does not stop reflux — but makes it less acidic and
feels more “comfortable”. We need to keep in mind that acid is the first defence against
14
food-borne bacteria/viruses! Essential minerals such as calcium, iron and zinc cannot be assimilated without the acid in the stomach and may be destroyed or compromised by drugs. Since zinc is connected to how well we can smell, as well as to “feeling hungry”, this will affect eating.
Common gastrointestinal disorders:
Reflux and esophagitis: Food comes up
Aspiration: Reflux causes irritation, acid going into airways, causing pneumonia. https://medlineplus.gov/ency/article/000121.htm — see aspiration pneumonia
Inflammation (eosinophilic esophagitis): Usually no reflux, but eosinophils cause an allergic reaction
Emptying of stomach: Influenced by stress and can lead to reflux. It is affected by the contents of the meal, the age of the child, the size of the meal, and how long the food stays in the stomach. Slow emptying — ”not hungry”; Rapid emptying (“Dumping syndrome”) can lead to nausea, vomiting, discomfort, bloating, cramping, diarrhoea, dizziness, fatigue, sweating.
Constipation: Caused by less fibre, dehydration. Suggested – use real foods
blended. Feels “full”. – appetite reduced.
Encopresis: Entire large intestines filled with faeces – resulting in pain and discomfort. If child strains, reflux can occur.
What are the responsibilities of feeding therapists? They need to understand:
That swallow mechanisms are a part of the gastrointestinal system
What gastroenterologists and other physicians are saying or suggesting, and know what questions to ask
Reports and suggestions from nutritionists — and ask questions
How the recommendations affect the child’s interest in food and learning eating
skills, and also their comfort level
Nutrition and hydration — and work with a dietitian to know how to incorporate powdered foods into preferred foods (e.g. yogurt)
The impact of stress on the gastrointestinal system, and learning how to calm a child (e.g., breathing, humming, imaging a favourite place, specific types of music)
And become familiar with alternatives to pharmaceutical solutions (eg sacral cranial therapy, cider vinegar, CALM powder). They need to not believe
everything they read, but read with “wise eyes” and look for evidence.
There are four main priorities to achieve “Inner directed” eating. Suzanne talks about the “4 Cs” of therapy: Connection, Comfort, Confidence, and Competence. I’m sure that these will resonate with us:
Connection: This is foundational to the other three. What is “connection”? This is about our relationships with the persons involved in feeding or at a meal. Does the person who is involved in the meal have a bond with the child? Does this person “listen” to the child’s voice or body language? Is there empathy? We know this — especially as we talk a lot about how an intervener (or others) need to first develop a bond with a child and have the child really trust him/her. We also know how to have “conversations” that do not use symbolic language, but rely on gesture, facial expression, body language and movement.
15
Comfort: Suzanne talks about three areas where “comfort” measures should be explored: gastrointestinal, sensorimotor, and emotional. I see those as interconnected — and can be complex to deal with. Often medical intervention, or therapeutic intervention is needed to patiently get children into this “comfortable” place. Often, especially with children who are tube-fed, there are both internal and external pressures on the child — dealing with the type of food, possible allergies, pain and discomfort while eating, too much food etc. There are a whole lot of other contributing factors to discomfort such as medication side-effects, surgical side-effects etc. The person feeding the child is also somewhat anxious — trying to figure out how much is “enough” or too much; how fast or slow to administer the food; what to do about medication changes, or simply how to help their child not experience stress. They are often going by what someone has told them to do, or what the can or container says, but do not know if this is what it really should be. The child may be losing weight, and so the parent feels pressure to feed more food. Real food that is blended has helped several children and families that I know — by reducing the discomfort a child feels, and also reducing tension in the parents. Another way to help with comfort is to regulate breathing, and what the brain is doing. Suzanne has used Hemi-sync technology successfully. See another brief article on this in this issue.
Confidence: Not only does a child have to develop trust and confidence in the person or persons involved in their feeding, but they must also trust what they are eating. If they are at all uncertain about the food, they will not be comfortable with it either. Think about yourself — if you find some new, strange food on your plate. You may react in one of several ways. You may outright reject the food because you don’t like changes or novel food. You may briefly taste it and reject it. You may throw a tantrum because it reminds you of something that repulses you. Also — ask yourself the question: How did I learn to eat some things that I originally did not like or have a taste for? You may have been influenced by another person. It is possible that you learned to like it slowly — and in small doses. And you may also have learned something more about the food — perhaps the nutritional value too. You also build confidence when you are not forced to eat something, but learn to do so willingly.
Competence: Something that has been tried, enjoyed, and repeated will have a child feeling that he is in control. Once this control exists, the mind and body become more relaxed and emotions are in control. This is truly when eating becomes “inner-directed”.
The notes above are my very brief ramblings — but if you can read the details in Suzanne’s blogs and other writings, you can read a whole lot more about this foundation for inner-directed mealtimes.
Some resources for you!
¨ Homemade Blended Formula Handbook: https://www.amazon.com/Homemade- Blended-Formula-Handbook- Marsha/dp/0615147127/ref=sr_1_5?ie=UTF8&qid=1484173650&sr=8-
5&keywords=suzanne+evans+morris
¨ Meal time Participation Guide: https://www.amazon.com/Mealtime-Participation-
16
Guide-Marsha- Klein/dp/076167408X/ref=sr_1_6?ie=UTF8&qid=1484173650&sr=8-
6&keywords=suzanne+evans+morris
¨ Marvellous Mouth Music: Songames for Speech Development: https://www.amazon.com/Marvelous-Mouth-Music-Songames- Development/dp/1935567098/ref=sr_1_4?ie=UTF8&qid=1484173650&sr=8-
4&keywords=suzanne+evans+morris and the CD too: https://www.autismcommunitystore.com/marvelous-mouth-music-cd-by-suzanne- evans-morris
(Kindly reproduced from the Oregon Deafblind Project Newsletter, Feb 2017)
1. Planning and starting the EHC Plan process
Contact your Local Authority (LA) Special Educational Needs (SEN) department to request for an EHC Plan assessment. The LA must respond to the request within 6 weeks saying if they will or will not carry out the assessment.
Once the LA has agreed to carry out the assessment they have 20 weeks to complete the process. The start date will be confirmed in writing along with information/forms about the assessment.
Your child should be assigned an SEN Advisory Officer. This person coordinates the EHC plan process. Do your best to get a good relationship going with your advisory officer.
Your advisory officer will ask you to give a list of health/educational professionals and therapists you wish to contribute to the EHC Plan.
o Contributors will be the health/educational professionals currently supporting your child. Include any private/independent professionals or therapists you are working with.
o There may be gaps in your child’s support; think of people or services you feel are needed to support your child. For example: support from a qualified MSI teacher or Occupational therapist. Ask your Advisory Officer to appoint any additional professionals/ therapists to contribute to the EHC Plan.
17
Examples of health/educational professionals & therapists who may be involved in supporting a child with Charge syndrome:
Qualified MSI teacher (MSI) Teacher of the Deaf (ToD) Visually Impairment Teacher (VI)
Specialist Hearing Impairment Speech and Language Therapist (SALT) Dysphagia Speech and Language Therapist (SALT)
Occupational Therapist (OT) Physiotherapist (PT) Educational Psychologist (EP)
Special Educational Needs Co-coordinator (SENCO) - based at school. Social Worker
Mobility Officer
Dietician
Health visitors
2. Assessments & Reports
All the health/educational professionals who contribute to the EHC Plan should do an assessment and produce a report for your child. The LA will provide a deadline for the reports.
Heath/educational professional reports:
o Should clearly state what support your child needs and why.
o Should avoid using language that can be misinterpreted.
o Quantify the amount of support your child will receive. (See below)
Ask to see the reports before the multi-agency meeting, this gives you time to
ask for amendments to be made.
You will also be asked to fill out an ‘All About Me’ form. A deadline will be
given to submit this form.
‘All About Me’ form:
o Keep language clear and to the point.
o Make sure you clearly state the help and support your child needs.
o List what works well and what is not working for you child.
o List your child’s strengths and weaknesses.
o Talk about the school environment you feels suits your child best and
why.
o Talk about current/future aspirations and wishes for your child.
If you are not happy with the support, assessments or reports produced by your local NHS health professionals/services, you can appoint an independent health professional to do an assessment/report. This can be added to the
EHC plan. Contact your advisory officer to let them know you want to submit an independent assessment/report.
This can be effective to help secure support for your child. Bear in mind that you need to pay for this (they can be expensive).
18
Submit any relevant reports from specialist consultant/doctors working with your child.
Examples of EHC Plan quantified support:
“Support from a qualified MSI teacher for a total of 26 hours over the academic year, the MSI teacher will work alongside the VI and HI teachers, provide on-going advice, teaching and support to take account of (child’s) multi-sensory needs. The time provided should include direct support to (child), to staff supporting/teaching and working with (child), as well as input for review of EHCP.”
“Advice and support from a Qualified Teacher for the Visually Impaired with a minimum of half termly visits, with access to the mobility officer and IT manager as appropriate.”
“The Speech and Language Therapist will carry out a number of visits over the school term that should total between 6 to 10 hours depending on the current need.”
“To meet the identified special educational needs of (child) she should receive support equivalent to the value of 32½ hours Intervener support (LSA trained to be intervener) which will be funded by the school and the Local Authority.”
3. Multi-agency meeting
All health & educational professionals who support your child should attend the meeting.
Independent professionals, therapists and organisations can attend the meeting. Sense are a very good support.
As there may be many professionals at the meeting ask your advisory officer to consider this and allow enough time for the meeting.
Make a list of what you would like to say at the meeting.
If you don’t agree with any of the reports, amount of support or services that
have been suggested, clearly communicate your concerns.
You may need to request for further assessments to be done after the meeting? This may delay receiving a draft plan.
It can be quite intimidating being in a room full of health professionals. Try to be brave, communication your concerns and let everyone know you will fight hard for your child. Don’t be afraid to be pushy – you are more likely to get what is needed to support your child.
4. Draft EHC Plan:
19
You have 2 weeks to accept or disagree with the prosed EHC plan.
Read though carefully and highlight/list any concerns you have.
Ask a couple of your health professionals to read through the proposed plan and give you advice on any changes needed. (Sense offers very good support).
Make sure the language is clear and support is quantified.
S.M.A.R.T goals should be included. (S.M.A.R.T goals: Specific, Measurable, Attainable, Relevant and Timely).
Don’t be afraid to disagree with the proposed plan. Don’t agree it until you are satisfied it meets your child’s needs.
5. Final Draft EHC Plan
Make sure all the health professionals and the school receive a copy of the
EHC plan final draft.
Make sure they read it!
Sometimes local NHS services do not meet the support written in the EHC plan. If this happens contact the manager of the service/s you are concerned about and your SEN advisory officer. Don’t take any nonsense - say you will take legal action if the ECH plan is not met.
Keep track of the support your child is receiving. Ask for a Home/School book where the support can be logged.
20
CHARGE Family Support Group Website http://www.chargesyndrome.org.uk
Steven Ho (Chair) Telephone: 07950 233100
Email: stivyh@gmail.com
Simon Howard (Vice Chair) Telephone: 020 8265 3604
Emails: si_howard@hotmail.com
Leanne Howie (Secretary) Telephone: 07804192868
Email: kit10grl@hotmail.com
The views expressed in this newsletter are not necessarily those held by the CHARGE Family Support Group.
21
INFORMATION SHEET![]()
Name of person with CHARGE
Address
Email address
Telephone No
DoB
Parent’s names
Address if different from above
Email address if different from above
Telephone No if different from above
Main Issues:
Please return to Simon Howard, 59 Elmer Road, London SE6 2HA or si_howard@hotmail.com
22
23

Posted on Wednesday 6 April 2022
CHARGE syndrome, which affects approximately one in 10,000 newborns worldwide, is associated with neurological and behavioural conditions like intellectual disability, attention deficit disorder, conv…

Posted on Tuesday 22 March 2022
A teenager who helped thousands of people learn British Sign Language (BSL) during the first Covid-19 lockdown is being turned into an animated character in new lessons.
Posted on Tuesday 11 January 2022
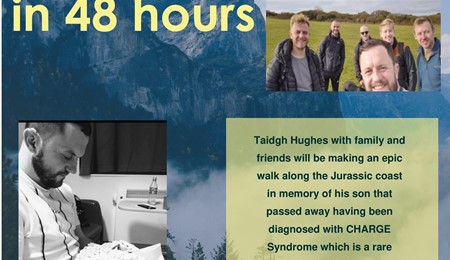
Taidgh Hughes with family and friends will be making an epic walk along the Jurassic coast in memory of his son that passed away having been diagnosed with CHARGE Syndrome which is a rare genetic dise…

Posted on Tuesday 8 December 2020
Study looking at a range of behaviours, skills and impairments in CHARGE syndrome.